Background: Urinary incontinence (UI) represents one of the most prevalent female intimate health issues negatively affecting a patients’ quality of life (QoL). Current treatment options require a combination of pelvic floor muscles exercising and intravaginal electrostimulation or drug treatment with side effects. Women seek non-invasive and efficacious solutions for UI.
Aim: The aim was to investigate the effect of High-Intensity Focused Electromagnetic technology (HIFEM) on QoL of incontinent patients.
Methods: 30 women (mean age 53.05 years) with stress, urge and mixed type of UI took part in the pilot study. They attended 6 therapies scheduled 2x a week. QoL was assessed through King’s Health Questionnaire (KHQ). The number of used hygienic pads and patients’ subjective feedback were recorded. Data was collected pre-, post-treatment, during 3- and 6-month follow-ups. KHQ scores were statistically evaluated through t-test (p<0.05). Number of used hygienic pads and patients’ subjective feedback were evaluated through frequency of occurence.
Results: After 6 treatments, 95 % of treated patients improved their QoL according to the scores of the KHQ. These results were maintained during the 3- and 6-month follow-ups. 67 % of the treated patients reduced or totally eliminated the use of hygienic pads in day-to-day life. 100 % of patients reported better awareness of the pelvic floor muscles.
Conclusion: Results suggest that the tested device significantly improves the QoL of incontinent patients.
Keywords: urinary incontinence, hygienic pads, King’s Health Questionnaire, Quality of Life, HIFEM technology, FDA.
1. INTRODUCTION
1.1.Definition of the problem : Urinary incontinence (UI) is involuntary loss of urine, which objectively and subjectively represents a social, psychological and hygienic problem. It is estimated that 1 in every 4 women aged between 30 and 59 years has experienced a problem with urinary leakage. Estimation of worldwide UI prevalence is around 40 % of the female population. However, a vast majority of the patients is reluctant to discuss this intimate issue with their medical doctors. National Association for Incontinence (NAFC) reports that 4.5 out of 10 patients do not seek help. (1, 11)
1.2.Types of urinary incontinence: UI can be divided into 3 types according to its’ etiology. Clinical symptoms of stress urinary incontinence (SUI) usually involve involuntary leakage of urine when events with increased intra- abdominal pressure are performed (e.g. coughing, sneezing, laughing and lifting). The cause of SUI is due to a loss of support of urethra and deconditioned pelvic floor musculature (PFM), which is usually a consequence of damage to the pelvic support structures. SUI is strongly associated with vaginal childbirth and menopausal hormonal changes (1). The second UI type is associated with a strong desire to void and pathological contractions of the bladder, so-called urge incontinence. Urge incontinence is a neuromuscular dysfunction commonly treated with pharmacotherapy. Urge incontinence is usually a symptom of an underlying problem (e.g. diabetes mellitus). The third UI type is mixed urinary incontinence (MUI) and involves a combination of the SUI and urge incontinence symptoms (1).
1.3 Treatment options for urinary incontinence: The choice of treatment for UI depends on its’ type and severity. In the case of SUI, treatment options range from pelvic floor muscle exercising, intravaginal electrotherapy up to surgical intervention. Surgical intervention is recommended usually only in severe cases of SUI, whereas drug treatment of urge incontinence is common. A vast majority of patients use hygienic pads and their quantity depends on the severity of UI and leakage episodes (13, 15).
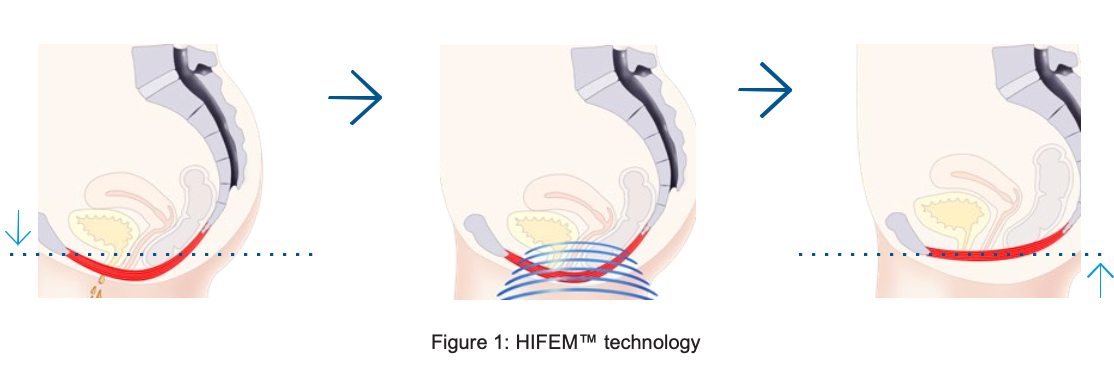
2. HIFEM technology
2.1.Mechanism of Action: High-intensity Focused Electromagnetic technology (HIFEM) triggers intense pelvic floor muscles contractions by targeting neuromuscular tissue and inducing electric currents. Electric currents depolarize neurons resulting in concentric contractions and lift up of all pelvic floor muscles. Key effectiveness is based on focused electromagnetic energy, in- depth penetration, and stimulation of the entire pelvic floor area. The HIFEM technology brings deep PFM stimulation and restoration of the neuromuscular control. The HIFEM passes non-invasively through pelvic floor area. Therefore, it represents a non-invasive solution for incontinent patients, who remain fully clothed during the therapy (2-10, 12, 14-19).
3. MATERIALS AND METHODS
3.1.Aim: The aim was to investigate the effect of HIFEM technology on QoL of incontinent patients. For such purpose 3 hypotheses were created:
- H0: Course of treatments with the HIFEM technology will not lead to any improvement of QoL of incontinent patients.
- H1: Course of treatments with the HIFEM technology will lead to significant improvement of QoL of incontinent patients.
- H2: Course of treatments with the HIFEM technology will reduce the use of hygienic pads.
3.2.Patients: All patients were enrolled in the pilot study after their voluntarily agreement and signed written informed consent. 30 women aged 36-76 years (mean age 53.05±11.74) with SUI, urge and MUI were included in the pilot study. UI resulted out as a consequence of vaginal childbirth, hormonal changes (menopause) or through obesity.
3.3.Exclusion criteria: Women with pacemakers, metal implants, blood coagulation disorders, tumors, fever, menstruation and pregnant women were not included in this study.
3.4.HIFEM technology tested device: In this pilot study, FDA approved device for female urinary incontinence treatment BTL EMSELLA (BTL EMSELLA, BTL Industries Inc.) was used.
3.5.Methods: The effect of HIFEM technology on QoL of incontinent patients was assessed through the King’s Health Questionnaire (KHQ). The KHQ detects incontinence impact in patients’ socio-emotional life and activities of daily living (ADL) (13). Additionally, number of used hygienic pads and patients’ subjective feedback were recorded.
4. COLLECTING THE DATA
4.1.Data collection Data was collected pre-, post-treatment and during 3- and 6-month follow-ups.
4.2.BTL EMSELLA therapy protocol: All women absolved 6 therapies scheduled 2x a week. Therapy was performed by medical personnel, who positioned the patient into a comfortable sitting position, feet on the floor, hip, knee and ankle joints perpendicularly flexed. 30-minute duration for each treatment session.
4.3.Therapy parameters: Frequency range 20-30 Hz with trapezoid intensity modulation was used to achieve gradual motor unit recruitment. Relative intensity (in %) was gradually increased from patients’ motor up to above the motor threshold.
4.4.Statistics: Data of 30 patients was collected and statistically evaluated. During the course of treatment no adverse events occurred and therapy was well tolerated. KHQ scores were calculated and tested for statistical significance by means of Student’s t-test at statistical significance level p<0.05. Improvements were compared as follows: between pre-treatment and post- treatment data, between pre-treatment and 3- and 6-month follow-ups data. Patients’ reports of the number of used hygienic pads were calculated as statistical frequency of occurrence between pre-treatment and post-treatment data, between pre-treatment and 3- and 6-month follow- ups data. Additionally, subjective feedback was collected from all patients. The frequency of answer occurrence was calculated.
5.RESULTS
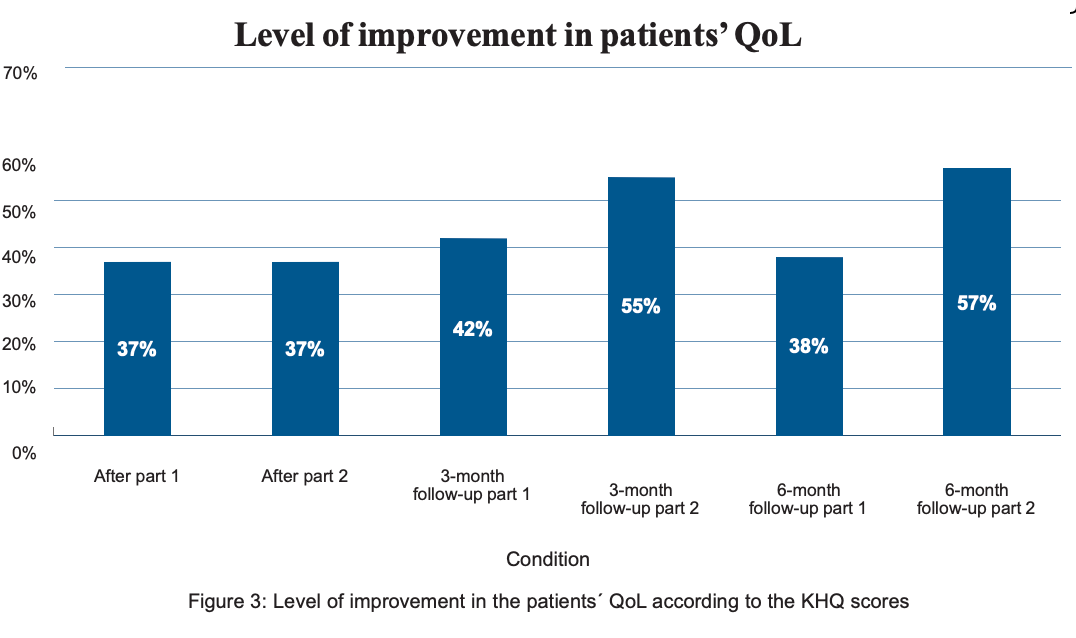
5.1The King’s Health Questionnaire results: The KHQ has two parts – Part 1 reports about the general health perception; Part 2 reports about the incontinence impact on the patient’s life. The scores are calculated separately. The research results proved/disproved following hypotheses and are discussed in the text below:
- H0: Course of treatments with the HIFEM technology will not lead to any improvement of QoL of incontinent patients.
H0 hypothesis disproved. All patients (n=30) have improved their QoL after a course of treatment with the HIFEM technology, which was proved by H1.
- H1: Course of treatments with the HIFEM technology will lead to significant improvement of QoL of incontinent patients.
H1 hypothesis proved. After the course of treatment with the HIFEM technology, 95 % of treated patients reported improvement in the QoL according to the scores of the KHQ. Before the therapy, the average score of the KHQ-Part 1 was 82.08 points. After course of treatment with the HIFEM technology, the average score of the KHQ-Part 1 was 51.67 points, which decreased to 45.42 points during 3 months and to 48.33 points during 6 months, respectively. These improvements are demonstrated as 37%, 42% and 38% levels of improvement in general health perception (p<0.05).
Before the therapy, the average score of the KHQ-Part 2 was 187.50 points. After a course of treatment with the HIFEM technology the average score of the KHQ- Part 1 was 103.75 points, which decreased to 81.11 points during 3 months and further to 74.44 points during 6 months, respectively. These improvements are demonstrated as 37%, 55% and 57% levels of improvement (p<0.05).
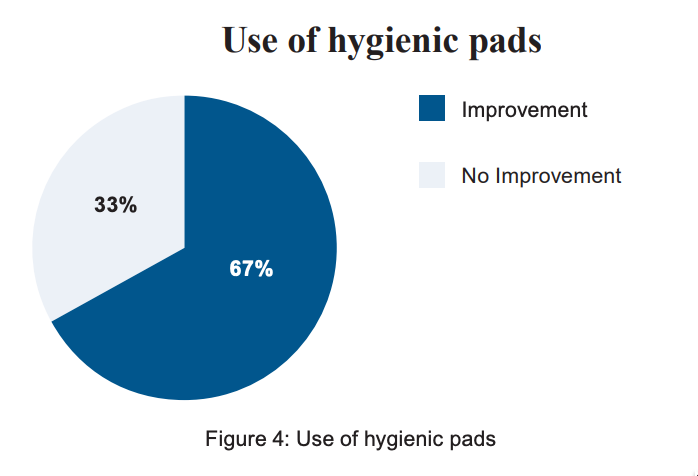
5.2The results of use of hygienic pads
- H2: Course of treatments with the HIFEM technology will reduce the use of hygienic pads.
H2 hypothesis proved. In this study, 12 patients wore hygienic pads during the day and night. Before the therapy, average number of used hygienic pads was 1.1 pad per day and night. After a course of treatment, 67 % (n=9) of treated patients totally eliminated or decreased the average number of used hygienic pads decreased to 0.45 pad per day and night. The results were maintained during the 3- and 6-month follow-ups.
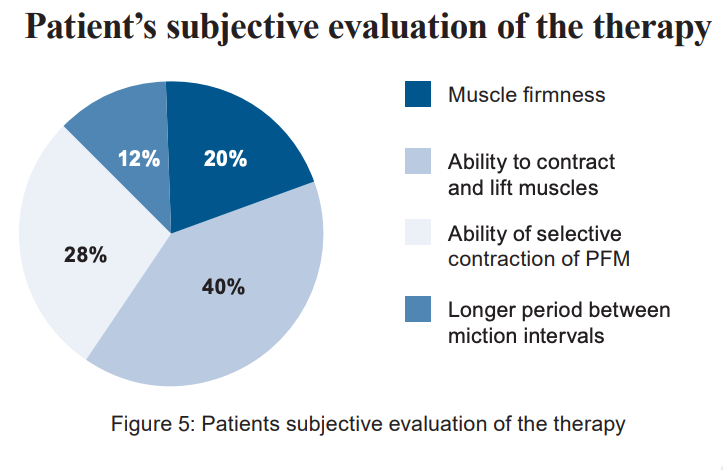
5.3. The patients’ subjective evaluation of the therapy: Additionally, patients answered the question ‘What is the major difference you noticed after the BTL EMSELLA therapies?’ 40 % of patients reported that they are able to perform proper contraction of the PFM; 28 % of patients were able to contract PFM selectively; 20 % of patients reported better muscle firmness and 12 % of patients reported that the period between micturition is longer. Additionally, all patients (n=30; 100 %) reported better awareness of pelvic floor muscles.
|
Parameter |
KHQ Part 1 |
KHQ part 2 |
|
KHQ score pre-treatment (Mean±SD) |
82.08±29.53 |
187.50±119.24 |
|
KHQ score post-treatment (Mean±SD) |
51.67±33.62 |
103.75±83.07 |
|
KHQ score, 3-month follow-up, (Mean±SD) |
45.42±26.83 |
81.11±64.94 |
|
KHQ score, 6-month follow-up, (Mean±SD) |
48.33±23.66 |
74.44±58.03 |
|
Level of improvement, Pre/Post-treatment |
37% |
37% |
|
Level of improvement, Pre-treatment/3-month follow up |
42% |
55% |
|
Level of improvement, Pre-treatment/6-month follow- up |
38% |
57% |
Figure 2: Results of the KHQ score
SD = standard deviation
6. DISCUSSION
To regain continence, regular pelvic floor muscles exercising is required. Normally, 300-500 contractions of the pelvic floor muscles should be performed to begin to develop a new motor pattern, whereas 3,000-5,000 contractions are required to erase and correct poor motor pattern. During 1 session using HIFEM technology, thousands PFM contractions are performed. This method is extremely important to PFM re-education as the patients are not able to perform this high-repetition rate pattern due to PFM weakness and an inability to consistently contract this muscle group. After 6 therapeutic sessions with HIFEM therapy, patients developed the new motor pattern needed to better control pelvic floor muscles and also regained muscle strength and continence control (3-9, 12-16).
7. CONCLUSION
UI represents a significant psycho-socio-economical healthcare problem that has a major negative impact on today’s modern lifestyles. The majority of patients are not satisfied with the current treatment methods offered, which include surgical intervention, drug therapy, pelvic floor muscles exercising (Kegel) or minimally invasive intravaginal procedures. This latest research, as well as, previous studies suggest that HIFEM technology leads to significant improvement in QoL of incontinent patients, maintains a patient’s privacy all while avoiding more invasive approaches.
8. CONFLICT OF INTEREST
Authors declare that no conflict of interest exists.
9. REFERENCES:
Abrams P, Blaivas JG, Stanton SL, Andersen JT. The Standardisation of Terminology of Lower Urinary Tract Function. The International Continence Society Committee on Standartisation of Terminology. Scand d Suppl 1998; 114:5-19
Abulhasan, J., Rumble, Y., Morgan, E., Slatter, W. and Grey, M. (2016). Peripheral Electrical and Magnetic Stimulation to Augment Resistance Training. Journal of Functional Morphology and Kinesiology, 1(3), pp.328- 342
Almeida FG, Bruschini H, Srougi M.: Urodynamic and clinical evaluation of 91 female patients with urinary incontinence treated with perineal magnetic stimulation: 1-year follow-up. J Urol. 2004 Apr; 171(4), pages 1571-4
Bickford, R., Guidi, M., Fortesque, P. and Swenson, M. (1987). Magnetic stimulation of human peripheral nerve and brain. Neurosurgery, 20(1), pp.110-116.
Bustamante, V., de Santa María, E., Gorostiza, A., Jiménez, U. and Gáldiz, J. (2010). Muscle training with repetitive magnetic stimulation of the quadriceps in severe COPD patients. Respiratory Medicine, 104(2), pp.237-245.
Coletti, D., Teodori, L., Albertini, M., Rocchi, M., Pristerà, A., Fini, M., Molinaro, M. and Adamo, S. (2007). Static magnetic fields enhance skeletal muscle differentiation in vitro by improving myoblast alignment. Cytometry Part A, 71A(10), pp.846-856.
Feldman M., Magnetic Stimulation for the Treatment of Urinary Incontinence in Women, California Technology Assessment Forum, San Francisco, CA, October 20, 2004
Han T.R., Shin H.I., Kim I.S. Magnetic stimulation of the quadriceps femoris muscle: comparison of pain with electrical stimulation. Am J Phys Med Rehabil 2006; 85(7):593-599.
Ishikawa N., Suda S., Sasaki T. et al., Development of a non-invasive treatment system for urinary incontinence using a functional continuous magnetic stimulator (FCMS) , Medical & Biological Engineering & Computing, 1998, 36, 704-710
Man, W. (2004). Magnetic stimulation for the measurement of respiratory and skeletal muscle function. European Respiratory Journal, 24(5), pp.846-860.
National Association for Incontinence (NAFC), www.nafc.org
Ostrovidov, S., Hosseini, V., Ahadian, S., Fujie, T., Parthiban, S., Ramalingam, M., Bae, H., Kaji, H. and Khademhosseini, A. (2014). Skeletal Muscle Tissue Engineering: Methods to Form Skeletal Myotubes and Their Applications. Tissue Engineering Part B: Reviews, 20(5), pp.403-436.
Sand PK, Richardson DA, Staskin DR. Pelvic floor electrical stimulation in the treatment of genuine stress incontinence: a multicenter, placebo- controlled trial. Am. J. Obstet. Gynecol. 1995; 173, pages 72–9
StÖlting, M., Arnold, A., Haralampieva, D., Handschin, C., Sulser, T. and Eberli, D. (2016). Magnetic stimulation supports muscle and nerve regeneration after trauma in mice. Muscle & Nerve, 53(4), pp.598-607. Truijen G, Wyndaele JJ, Weyler J.: Conservative treatment of stress urinary incontinence in women: Who will benefit? Int Urogynecol J Pelvic Floor Dysfunct. 2001; 12(6), pages 386-90
Wallis, M., Davies, E., Thalib, L. and Griffiths, S. (2011). Pelvic Static Magnetic Stimulation to Control Urinary Incontinence in Older Women: A Randomized Controlled Trial. Clinical Medicine & Research, 10(1), pp.7- 14.
Yamanishi T, Yasuda K, Suda S et al. Effect of functional continuous magnetic stimulation for urinary incontinence. J. Urol. 2000; 163, pages 456–9
Yamanishi T, Yasuda K, Sakakibara R et al. Pelvic floor electrical stimulation in the treatment of stress incontinence: an investigational study and a placebo controlled double- blind trial. J. Urol. 1997; 158, pages 2127–31
Yang, S., Jee, S., Hwang, S. and Sohn, M. (2017). Strengthening of Quadriceps by Neuromuscular Magnetic Stimulation in Healthy Subjects. PM&R.
Berenholz J., MD1, Sims T., MD2, Botros G., MD2
Affiliations:
1The Laser Vaginal Rejuvenation Institute Of Michigan Farmington Hills, MI, USA
2The Medical Laser and Aesthetics Group, Wirral, United Kingdom